For many years, cryopreservation has been the primary technique for conserving biological specimens.
It has enabled researchers to answer new research questions using rare or valuable samples from decades ago.
It’s now used to store and distribute biological treatments and preserve the most recent complex cell models for future use by other scientists.
In this article, Dr. Hrishikesh Pai from Babies & Us Fertility IVF & ICSI Centre, the excellent IVF center in Mumbai, explores the challenges of cryopreservation and the emerging advances that could improve these methods.
What is cryopreservation?
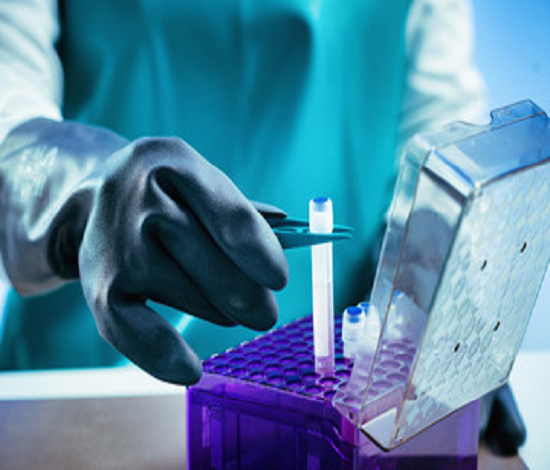
Cryopreservation involves tissues, freezing cells, organs, or additional biological materials at low temperatures. Cryo is the Greek word for “freeze.”
The most common method in research labs is to freeze samples at –80 °C using solid CO2 or –196 °C using liquid nitrogen.
However, a vitrification method is used for the long-term storage of clinical samples such as sperm, fertilized eggs, or ovarian tissue.
The main distinction is that conventional cryopreservation techniques let ice form during the preservation procedure, whereas vitrification solidifies the real solution without ice crystallization.
Applications of cryopreservation
Traditional cryopreservation, which works by keeping cells in “suspended animation,” is a highly effective method for storing cells and tissues.
The metabolic activity of cells is stopped when they are frozen, and the compounds within them, such as enzymes, are preserved.
It would help keep cells and tissues alive in continuous culture without cryopreservation, which means growing and splitting them to generate more cells (called passaging).
On the other hand, cells change as they multiply, which can result in them losing essential characteristics.
The heterogeneity that would otherwise be introduced by repeatedly passaging them is reduced by freezing them.
Dr. Hrishikesh Pai, a leading Infertility specialist from India, says, “From our perspective, cryopreservation allows us to bank new cellular models for the research community, which people can refer to for years to come.”
It means we can keep the model for a long time, but the cells aren’t constantly dividing to the point where they’ve mutated to look like the cells you started with.
The rapidly emerging field of cell-based therapies, such as preserving mesenchymal stem cells for transplant or chimeric antigen receptor T cells (CAR T cells) for cancer treatment, is one area where cryopreservation is getting increasingly essential.
T cells from a patient are removed, re-engineered to recognize antigens (such as tumor-associated antigens), and then returned with CAR-T cell therapy.
“You have to do a lot of processing on these cells, possibly moving them between sites, getting them from the patient when they donate them to the lab, and then getting them back to the patient,” Dr. Hrishikesh Pai, an excellent IVF specialist from Mumbai explains.
“Treatments like these should ideally be frozen in a format that allows them to be quickly thawed and administered to patients at the bedside.”
When you have to do a lot of processing in a hospital setting, it becomes a barrier, and all of these steps add up to a lot of money.
“Anything that makes the procedure efficient and results in the patient acquiring more beneficial cells back after freezing is useful for the patient.”

Cryopreservation’s Limitations.
The cell recovery rate after freezing is among the primary constraints of current cryopreservation techniques.
And while you might have time to wait for your cells to multiply while working on a research project, you won’t be able to do so for clinical applications like the ones mentioned above.
Ice crystals form within the sample during the freezing process, damaging the cells, and some of the cells never recover.
According to Dr. Hrishikesh Pai, an expert IVF specialist from Mumbai, in most lab and clinical protocols, cryoprotectants or controlled rate freezing and thawing are used to protect cells from ice crystals and avoid shocking the cells with sudden temperature changes.
Many different cryoprotectants are available, but dimethyl sulfoxide is the most common cryoprotectant used for mammalian cells and tissues (DMSO).
Glycerol is another option for bacterial cells and red blood cells.
However, cryoprotectants have drawbacks; DMSO is the best protectant, but it is toxic to cells at specific concentrations.
Glycerol is gentler on cells than DMSO, but it is less effective as a cryoprotectant.
Using various blends of cryoprotective agents, like supplementing a lower concentration of DMSO with polypropylene glycol or glycerol, is one way to mitigate potential toxicity issues.